
Jumping into the Black Hole…
Space, it’s the final frontier. Since 1961 when the first humans entered space, we’ve been curious about it’s potential. Will the moon become the next hot tourist destination? Could militarization of space be possible? What about colonization of another planet? However, to address any of these questions, we first need to confidently answer the question “can we even survive space?’ Many studies have been done on the impact of spaceflight on the human body, from bone mass and biochemistry to changes in the signaling system within the brain. However, apart from a small portion of the NASA Twins Study (more information on this study here), very little research has been conducted on the effects of spaceflight on the microbiome. In recent years the human microbiome, or collection of all microbiota living within and on our bodies, has been at the forefront of medical research and researchers are now able to link changes in the microbiome with diseases like diabetes, inflammatory bowel disease, and preterm birth (The iHMP Research Network Consortium 2014).
For the first time, researchers (Voorhies et al. 2019) have published data tracking the microbiome of astronauts during long-term space missions. Researchers were curious if any changes occurred in the microbiome of astronauts onboard the closed environment of the International Space Station (ISS). They predicted diversity and abundance in the gut and on the skin would diminish while in space due to the sterile environment and limited diet.

Eclipsing Our Predictions…
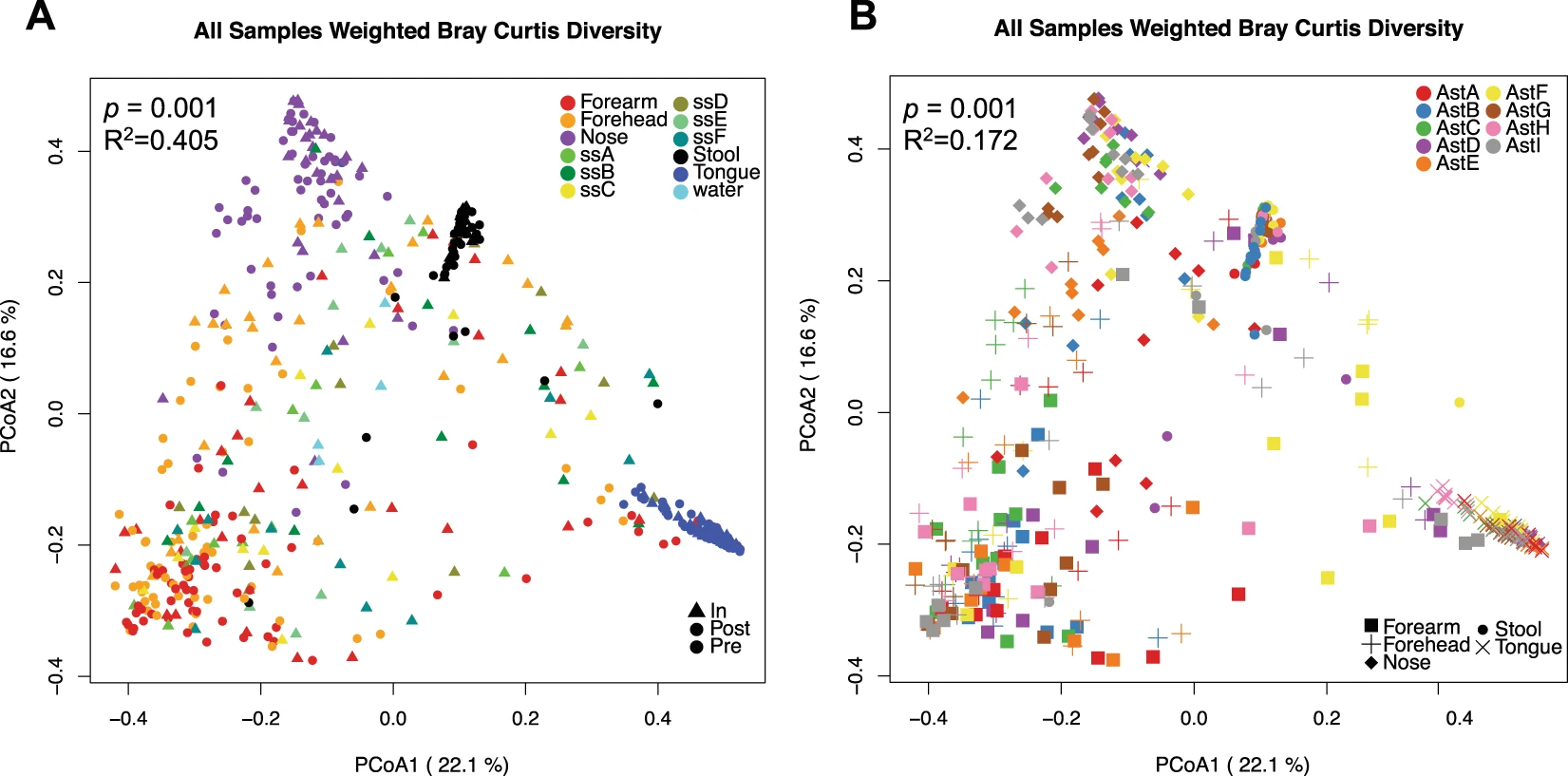
Voorhies et al. followed nine different astronauts into space for anywhere from 6 months to a full year’s mission at the ISS. Astronauts took samples of their microbes on their forehead, forearm, tongue, nostrils, and five of the astronauts took stool samples to represent the microbes living within their guts.
Researchers found that four out of the five astronauts experienced an increase in both diversity and abundance of the gut microbiota while in space. However, it’s important to note that an increase in diversity and abundance does not mean an increase in health. While increased microbiome abundance and/or diversity coinciding with better health is a pattern often seen in microbiome research, we must be cautious to assume the same pattern is occurring here in space. Some of the newly occurring microbes researchers identified have also been associated with the production of signaling molecules that cause inflammation (Crucian et al. 2014). Surprisingly, a single astronaut experienced no change to his gut microbiota in space. This same astronaut also had the highest diversity and abundance going into the mission, suggesting that a well-developed GI microbiome could be a good defense against the disruption space travel brings.
Microbiota changes of the forehead and forearm were inconsistent within the group, suggesting that personal factors like skin moisture, pH, and hygiene habits could have different reactions to space travel. However, all astronauts had a significant decrease in Gammaproteobacteria, a group of medically important bacteria, which have been hypothesized to be an explanation as to why skin rashes and infections are the most commonly reported symptoms by astronauts. A previous study found that individuals residing in areas with abundant amounts of agriculture had a higher abundance of Gammaproteobacteria (Ruokolainen 2014). Lack of these types of environments in the ISS could account for their drop in these bacteria and therefore increased skin reactivity.
Researchers also took blood and saliva samples to compare hormone levels and virus reactivation to the changes in the microbiome to see if any sort of correlation existed. Virus reactivation occurs when a dormant virus begins to start reproducing. Although none of the astronauts experienced any virus symptoms, four astronauts had a specific virus, Varicella-zoster, the cause of chickenpox and shingles, reactivated by flight day 90. Due to none of the astronauts reporting any symptoms of the virus, it’s unclear as to whether these findings are considered relevant. Researchers were also looking for changes in three different stress hormones: alpha-amylase, cortisol, and DHEA. Hormones are a type of signaling molecule produced by the brain that help to determine our behavior and physiology. By the second half of the mission a significant increase was detected in alpha-amylase, a hormone associated with social stressors (Petrakova et al. 2015) and a marker for the sympathetic nervous system, the unconscious part of the nervous system that controls our ‘fight or flight’ response (Mandsager 2015). Researchers are still unsure as to whether this increase is due to astronauts experiencing severe isolation, an increase of sympathetic nerve activity, or a combination of the two. Researchers also detected a decrease in DHEA. In previous studies, low levels of DHEA have been associated with Chronic Fatigue Syndrome (Becker et al. 1999). Researchers were surprised to find no change in cortisol levels during space flight, as other studies have previously found an increase in this stress hormone (Pierson et al. 2005).
Researchers additionally had the astronauts take samples from six different surfaces on the ISS in order to see what effects the environment might have had on the astronauts’ microbiome. They found the microbiome of the forehead and forearm more similar compared to these environments and surprisingly that the astronauts had more impact on the microbiome of the surface than the surface had on the astronaut. Because only 6 astronauts can be onboard the ISS at a time, frequent changes of crews occurred at the ISS during the experiment. As one crew left and another arrived, the samples from the ISS surfaces would more closely resemble the skin microbiomes of it’s new crew. Researchers did however find a core group of microbiota that were present in all samples and are unsure if this core group is native to the ISS or is simply the most common microbiota on human skin.
Looking through the Nebula…
This research brought up so many new and different questions that constitute its own research. Research could be done specifically on the GI microbiome of the astronaut that experienced no change and what made theirs so resilient compared to the other astronauts. Because of the large proportion of in-space skin rashes, the link between specific microbiota and it’s mechanisms that contribute to higher production of pro-inflammatory cytokines and the role of Gammaproteobacteria would be another area deserving of more in-depth research. Research conducted on virus reactivation during spaceflight and whether longer space duration results in virus symptoms in the astronauts is another question that would provide important answers to the central question of this study. Research expanding on these topics could help us to develop procedures that could minimize or maybe even diminish microbiome changes between terrestrial and celestial environments. Another point to acknowledge is this research had an incredibly low sample size, with only nine astronauts participating and even fewer participants involved in stool collection (n=5). This experiment conducted again at a larger sample size would yield even more data that could be useful in predicting average changes in the human microbiome in space.
Astronomically Curious about Astronomy…
- Interested in how the kind of data was collected? Check out this video by NASA about their Microbial Tracking Series
- For more information on this type of research, check out this video interviewing senior scientist at NASA’s Johnson Space Center, Dr. Cherie Oubre
- To learn more about the microbiome portion of NASA’s Twin Study, check out this informative video
Reference the Stars…
- Becker, P. De, et al. “Dehydroepiandrosterone (DHEA) Response to I.v. ACTH in Patients with Chronic Fatigue Syndrome.’ Hormone and Metabolic Research, vol. 31, no. 01, 1999, pp. 18—21., doi:10.1055/s-2007-978690.
- Crucian, Brian E., et al. “Plasma Cytokine Concentrations Indicate That In Vivo Hormonal Regulation of Immunity Is Altered During Long-Duration Spaceflight.’ Journal of Interferon & Cytokine Research, vol. 34, no. 10, 2 Oct. 2014, pp. 778—786., doi:10.1055/s-2007-978690.
- Mandsager, Kyle Timothy, et al. “The Function of the Autonomic Nervous System during Spaceflight.’ Clinical Autonomic Research, vol. 25, no. 3, 2015, pp. 141—151., doi:10.1007/s10286-015-0285-y.
- Garrett-Bakelman, Francine, et al. “The NASA Twins Study: A Multidimensional Analysis of a Year-Long Human Spaceflight.’ Science, vol. 364, no. 6436, 12 Apr. 2019, doi:10.1126/science.aau8650.
- Petrakova, Liubov, et al. “Psychosocial Stress Increases Salivary Alpha-Amylase Activity Independently from Plasma Noradrenaline Levels.’ Plos One, vol. 10, no. 8, 2015, doi:10.1371/journal.pone.0134561.
- Pflughoeft, Kathryn J., and James Versalovic. “Human Microbiome in Health and Disease.’ Annual Review of Pathology: Mechanisms of Disease, vol. 7, no. 1, 2012, pp. 99—122., doi:10.1146/annurev-pathol-011811-132421.
- Pierson, D.l., et al. “Epstein—Barr Virus Shedding by Astronauts during Space Flight.’ Brain, Behavior, and Immunity, vol. 19, no. 3, 2005, pp. 235—242., doi:10.1016/j.bbi.2004.08.001.
- Ruokolainen, L. “Green Areas Around Homes Reduce Atopic Sensitization in Children.’ Pediatrics, vol. 136, no. Supplement, 2015, doi:10.1542/peds.2015-2776x.
- Voorhies, Alexander A., et al. “Study of the Impact of Long-Duration Space Missions at the International Space Station on the Astronaut Microbiome.’ Scientific Reports, vol. 9, no. 1, 2019, doi:10.1038/s41598-019-46303-8.
- The iHMP Research Network Consortium. “The Integrative Human Microbiome Project: Dynamic Analysis of Microbiome-Host Omics Profiles during Periods of Human Health and Disease.’ Cell Host & Microbe, vol. 16, no. 3, 2014, pp. 276—289., doi:10.1016/j.chom.2014.08.014.
