What is Fibromyalgia and who does it affect?
Could you imagine waking up every day with pain that never goes away? That is the reality many fibromyalgia sufferers experience in their everyday lives. Fibromyalgia is from the Latin word fiber (fiber) and the Greek words myo (muscle) and algos (pain). These root words offer a glimpse into what fibromyalgia is and how it causes suffering. It is a pain of the fibrous tissues and muscle in the human body. While anyone of any background regardless of race or ethnicity can get fibromyalgia, it typically affects women more than men (NIH, 2024). You are more likely to develop fibromyalgia as you age, and if a family member has fibromyalgia. There are cases of children and young adults having fibromyalgia, but it usually occurs in middle-aged women (Erdrich et al., 2023).
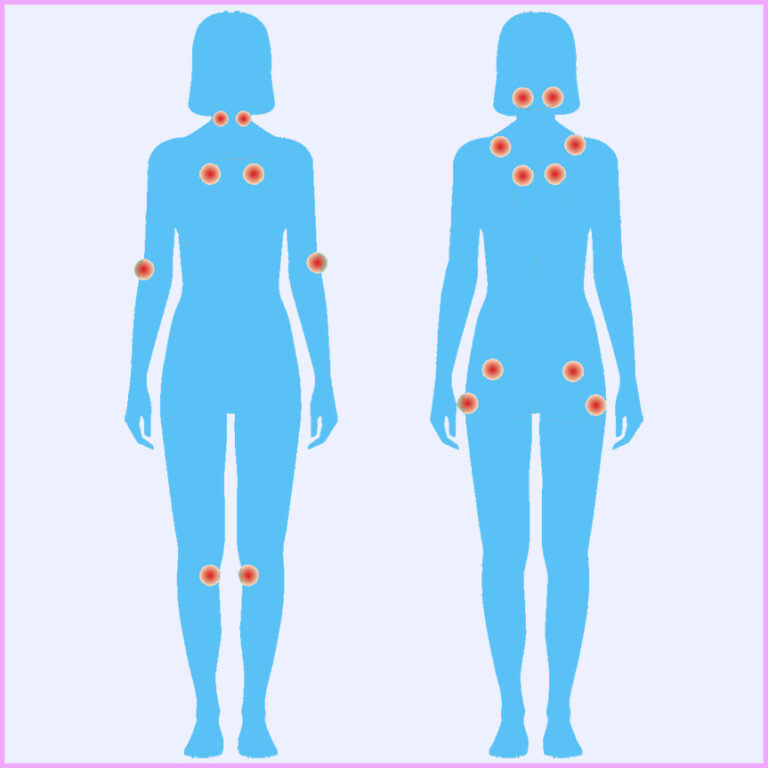
Around 2 to 4% of adults live with the challenges of fibromyalgia (Stewart, 2022). They wake up, feeling exhausted, struggling to get through daily tasks, and facing unpredictable flare-ups. This chronic condition, along with many other symptoms mentioned can affect your mental health, sleep and cognitive issues like brain fog, chronic headaches, and memory impairment. In addition, It can also make you more at risk for depression and anxiety by more than 50% (Freirich et al., 2021). Figure 1(A) displays many of the possible or common symptoms that sufferers of fibromyalgia have. The National Institute of Health has a great page about fibromyalgia, including its symptoms, causes and an overview.
Fibromyalgia is also frustrating to many patients and clinicians because it does not have defined diagnostic criteria that is 100% accurate. Clinicians in many fields of medicine such as neurology, rheumatology, psychiatry, and pain management have looked at this disease and now they are looking at the gut microbiomes. Many patients self-report symptoms and normally this is how clinician determine they have this illness. There are specific focal points that clinicians look for with their diagnostic criteria (Fig. 1B) There are a total of 18 points on the body that are painful and to diagnose fibromyalgia at least 11 of them must be reported by the patient (Moglia, 2024). From there, a clinician usually rules out any other causes that could mimic these symptoms. Since it tends to mimic different diseases like lupus, multiple sclerosis, rheumatoid arthritis, chronic fatigue syndrome, and more. There is no set diagnostic criteria to diagnose Fibromyalgia causing frustration with patients and clinicians, and leads to inaccurate diagnoses. Clinicians may use a fibromyalgia diagnosis as an “I don’t know what’s wrong with you” diagnosis. The estimated percentage of false positives is around 66% to 73% (Minerbi et al., 2019). Studies have shown connections between the microbiome and fibromyalgia patients A systematic review found that people with fibromyalgia have imbalances in their gut bacteria, which can affect their health. This imbalance, known as dysbiosis, may lead to increased gut permeability and heightened pain sensitivity (Palma-Ordonez et al., 2024).
Central question
How is the gut microbiome different between fibromyalgia patients and healthy individuals, and how are these differences related to fibromyalgia symptoms?
Where is the evidence?
In one study, they performed a lactose hydrogen breath test. This test is normally used to diagnose lactose intolerance by measuring the hydrogen in the breath of someone after they consume milk. In this study, they observe if there was an overgrowth of bacteria in the small bowels of fibromyalgia patients. Resulting in a 100% bacterial overgrowth in fibromyalgia patients while only observing a 20% bacteria overgrowth in the control patients (Minerbi & Fitzcharles, 2020).
New research into possible links between the microbiome and fibromyalgia.
How does the gut microbiome of individuals with fibromyalgia differ from those who are healthy? Is there a relationship between symptoms of fibromyalgia and altered gut microbiome? New research may help link gut microbiota to different disease processes like fibromyalgia. A recent study took place at the Allen Edwards pain management unit, and the West island rheumatology clinic by (Minerbi et al., 2019). This study looked into the possible interaction of the gut microbiome, and the central nervous system. This “gut-brain axis” may prove the link that the gut microbiome can affect the nervous systems processing and perception of pain (Minerbi et al., 2019). The study looked for participants with fibromyalgia, female and age 30 to 60 years old. They also recruited a group of healthy individuals or “controls” meeting the criteria of men and women aged 30 to 70 years old , and healthy women ages 30 to 60. They excluded anyone with other major, chronic illnesses, those who had an acute illness in the month before, and anyone who had taken antibiotics in the two months before. They also excluded anyone who had extreme dietary changes in the month preceding.
The studies diagnostic criteria, such as severity, pain, location, cognitive, disruptions, sleep, problems, and fatigue in addition to looking at the diagnostic criteria they also evaluated the impacts of fibromyalgia. They looked at any difficulty with pain, fatigue, tiredness, stiffness, anxiety, depression, and difficulty working as well as physical activity and sleep quality (Minerbi et al., 2019). The participants were asked to collect a stool sample and deliver it for processing. From the samples of stool they did genetic testing for the different bacteria by looking at the 16s region, a small part in the genes of bacteria. The 16s region is a sequence that stays similar across many species and is used to study how different organisms are related and used to help identify bacteria.
The key findings of the study were that they identified over 1600 types of bacteria or OTUs (operational taxonomic units) in the stool samples. The analysis of the got Microbiome composition had significant alterations present in fibromyalgia patients. 13 OTU showed higher abundance in fibromyalgia patients and 5 in the controls. Notably, species such as Parabacteroides merdae and Clostridium scindens were more prevalent in FM patients, while Prevotella copri and Bacteroides uniformis were less abundant. This is just a fancy way of saying there is a disturbance in the microbiota of fibromyalgia patients compared to the control’s (healthy peoples) microbiota. They also ran the results through a machine, learning algorithm, Lasso and SVM. This algorithm system of learning used 90% of the information as training and 10% testing for multiple rounds. This learning algorithm was able to start predicting a diagnosis of Fibromyalgia This algorithm showed accuracy of 87% for identifying fibromyalgia patients by their gut Microbiome. This could be a way for a future diagnostic exam to help clinicians identify if someone has fibromyalgia or not.
Certain microbes in our body are known for their anti-inflammatory properties, and these were found depleted in fibromyalgia patients. This could contribute to the inflammatory pain related symptoms of the condition. This is shown in Figure 2, where the X axis represents the abundance of bacteria and the Y axis lists different factors of fibromyalgia patients in the study. The heat map colors are the strength of the relationship between the two axis. Blue shades mean a positive correlation where high bacteria levels are linked to more severe symptoms. Red shades show a negative correlation where higher bacteria levels are linked to less symptoms. The small black dots within these colors represent statistically significant correlations. This heat map tells us that certain gut bacteria may be associated with the severity of symptoms and it is highlighting the role of the gut microbiome in understanding fibromyalgia.
The results of the study showed that there was a small difference in the diversity of the microbiota between the fibromyalgia patients and the controls. However, the abundance of certain microbiota in the microbiome of fibromyalgia patients was significantly different. Even more interesting is that the severity of symptoms correlated with specific Microbiome alterations (Minerbi et al., 2019).
My question
Is there a possibility for Diagnostic criteria in the gut?
With this new research, there is hope for a diagnostic test to diagnose fibromyalgia, and maybe even other similar diseases like irritable bowel syndrome or chronic fatigue syndrome. More research is needed in this field of study as most of it is relatively new within the last couple of years. A larger diversity of fibromyalgia patients should be explored, including younger adults, different ethnicities, and male participants. Hopefully with further studies we can understand the human microbiome and disease processes they may be linked to.
Further Reading
If you are interested in further reading about fibromyalgia and the gut microbiome, I would recommend this study. This study is about investigating the association between the symptoms of women with Fibromyalgia, Digestive function, and markers of the microbiota of the Gastrointestinal Tract (The FIDGIT Study). Another interesting study i recommend is An association between chronic widespread pain and the gut microbiome. This study looks at the link between chronic widespread pain (like fibromyalgia) and a a lower microbial diversity in the gut microbiome.
References
