Understanding the role of microbes in our environment and how antimicrobial resistance and hospital acquired infections are spread in the healthcare environment are some of the highlights of modern science.
Our new environment
People living in the United States spend 90% of their time indoors (Klepeis et al 2016). We live in our homes, work in our office buildings, and spend recreational time in the gym. One such common indoor environment- where we are born, and get treated for illnesses- is the hospital. How has this shift into the indoors impacted human health? Studies have linked this new environment to diseases like asthma and allergies (Fujimura et al 2014). In 2011, there were an estimated 722,000 hospital acquired infections in the U.S. (Magill et al 2014). And these infections- termed nosocomial infections- are reported as a leading cause of patient deaths (Anderson 2002).
Another growing healthcare concern is the propagation of antimicrobial resistance. Microbes can develop methods of combating the drugs that had once successfully inhibited them. As a result, typical drug treatments become useless, infections persist and may spread to others. This resistance is facilitated by genes that encode mechanisms for drug negation. and these genes can be transferred among microbial communities.
So why are these new disease trends being seen? One hypothesis says that as we shift from outdoor to indoor environments, our interactions with microbes also shift (Blaser and Falkow 2009). Specifically, the emphasis on antibacterial living styles has contributed to lessened microbial contact. Researchers now suggest that this loss of interaction is not beneficial to humans (Blaser and Falkow 2009).
To combat these concerns scientists have begun to describe the system that encompasses us, our environment, and the microbes living throughout that environment. Considerable work has begun to understand the transit of microbes between building and building occupants and thus facilitate a movement towards construction of buildings that promote human health.
What is the Plan?
As the demand for answers to these problems have increased, dedicated projects have quickly assembled to constitute the supply. One such project was the Hospital Microbiome Project, first convened in June 2012. Around this time, the University of Chicago was in the process of constructing a new hospital, the Center for Care and Discovery. Lax et al took the opportunity presented from a newly built, never before occupied hospital, to take a survey of surfaces, air, staff and patients from both before and after hospital opening (Lax et al 2017). Researchers wanted to understand the community-level spread and colonization of bacteria in a healthcare environment and how abiotic factors influence this transmission.
The Hospital Environment
Microbial communities found on hospital surfaces were clearly differentiable between samples taken before opening and after opening. Floors and surfaces converged to bacterial types associated with human skin. This clear shift is demonstrated from an analysis of OTUs identified before and after hospital opening.
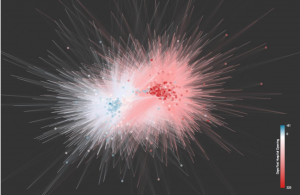
Figure1: Distance in this figure represents relatedness of bacterial taxa- very close points are similar, those that are farther apart are less related. Two epicenters (red on the right, blue on the left) show a clear shift in operational taxonomic unit composition of pre-opening and post-opening hospital surfaces (S2 of Lax et al 2017).
The strongest finding from this longitudinal hospital study showed that patient’s rooms were colonized by the microbes from the patient. However, during the first day of hospital stay, the bacterial community representative of the room transferred to the patient. So, before there was enough time for the patient to spread their signature bacterial mark on the hospital room, the vector of bacterial transfer was from room to patient.
Further analysis, extracted from whole genome sequencing of all bacteria found in samples showed that antimicrobial resistance genes were much more common to be found on the hospital surfaces than on the patients of the respective rooms. Some specific bacterial genera were prevalent and found throughout. This included Staphylococcus and Propionibacterium, genera which include pathogenic species correlated with common hospital acquired infections.
This study also explored the effect of environmental conditions on microbial transmission. However, there were no strong relationships identified between microbial transmission and the abiotic factors that researchers measured. These included temperature, relative humidity, and illuminance. Of the myriad of clinical factors investigated, a few relationships stood out. For example, patients that were admitted to the hospital through the emergency department saw lower diversity in their microbiomes. Additionally, chemotherapy patients had significantly less microbial diversity on their hands, in their nose, and on their bed rails.
What is Next?
Lax et al presented a solid foundation of data in his study of the hospital environment and the people and microbes within. Specifically, we saw that there is considerable exchange of microbes between patient and patient room. Troublesome genes that can confer antimicrobial resistance were much more likely to be found on surfaces than on patients. Beyond these results, their research has opened the door to further studies that will describe and characterize our built environments.
Undoubtedly, more information must be presented about the specific virulence, antimicrobial resistance, or functions that surround the microbes harbored in healthcare environments. Understanding what microbes are living in and around us is the first step. Next, more thorough sequencing will tell what these microbes do and if they are harmful to us through pathogenic features.
This research did not find large significance in any abiotic conditions as a factor of microbial transmission. These negative results could be a because there truly is no influence contributed by the factors measured. But it is also possible that other variables may have masked abiotic factor influence. To compare, an effect like temperature induces greater microbial growth which could plausibly induce greater transmission of microbes. Either way, there has not been extensive research done on these ideas and these results should be validated further before nullifying the effects of abiotic conditions. Additionally, this research presented a sample size of only one location. More location sites- providing variety in location and greater sample size- should be incorporated to allow for telling evidence that factors like humidity or illuminance are truly negligible for how microbes move around us.
To incorporate the regard for human health into our built environment there is a need to survey what types of building materials are most prone to harboring microbes. Questions that should be asked include what kind of materials or building surfaces are most prone to cultivating bacterial growth. Does the growth of pathogenic bacteria appear to be enhanced for one type of building surface when compared to another? Do specific surfaces facilitate the transfer of antimicrobial resistance genes between microbes? Creating an index of the microbial properties of our building surfaces will bring science one step closer to understanding the built environment and its role in microbial transmission.
While our lives have been undeniably impacted by the time we spend indoors we don’t have to let this impede on human health. Science is breaching new fields and topics for understanding what these changes mean for disease transmission and human microbiomes. The near future will see solutions to these questions.
Further Reading
The microbiome of the built environment is a flourishing field full of information. Check out some of the projects and research dedicated to understanding this topic:
- Here is another publication by the author of the research discussed in this post. This touches on hospital acquired infections specifically: Hospital-associated microbiota and implications for nosocomial infections
- This website discusses more details on the University of Chicago’s new hospital and the study conducted. https://hospitalmicrobiome.com/
- The Earth Microbiome Project is an extensive world-wide collaboration of microbial community sequencing- the Hospital Microbiome Project is a participant in this study. https://www.earthmicrobiome.org/
- The Microbiome Project: Hospitals– A youtube video that presents the reasoning of the hospital micro biome study
References
- Klepeis N, Nelson W, Ott W, Robinson J, Tsang A, Switzer P, Behar J, Hern S, Engelmann W, Nelson W, Ott W…, Journal of exposure analysis and environmental epidemiology, vol. 11, issue 3,pp. 231-52 Published by American Society for Microbiology Journals (2016). 10.1038/sj.jea.7500165
- K. E. Fujimura, T. Demoor, M. Rauch, A. A. Faruqi, S. Jang, C. C. Johnson, H. A. Boushey, E. Zoratti, D. Ownby, N. W. Lukacs, S. V. Lynch, House dust exposure mediates’¨gut microbiome Lactobacillus enrichment and airway immune defense against allergens and virus infection. Proc. Natl. Acad. Sci. U.S.A. 111, 805—810 (2014). 10.1073/pnas.1310750111
- Magill S, Edwards J, Bamberg W, Beldavs Z, Dumyati G, Kainer M, Lynfield R, Maloney M, McAllister-Hollod L, Na …see all
The New England journal of medicine, vol. 370, issue 13 (2014) pp. 1198-1208. 10.1056/NEJMoa1306801 - R. N. Anderson, B. L. Smith, Deaths: Leading causes for 2002. Natl. Vital Stat. Rep. 53, 67—70 (2002).
- M. J. Blaser, S. Falkow, What are the consequences of the disappearing human microbiota? Nat. Rev. Microbiol. 7, 887—894 (2009). 10.1038/nrmicro2245
- S. Lax, N. Sangwan, D. Smith, P. Larsen, K. M. Handley, M. Richardson, K. Guyton, M. Krezalek, B. D. Shogan, J. Defazio, I. Flemming, B. Shakhsheer, S. Weber, E. Landon, S. Garcia-Houchins, J. Siegel, J. Alverdy, R. Knight, B. Stephens, J. A. Gilbert, Bacterial colonization and succession in a newly opened hospital. Sci. Transl. Med. 9, eaah6500 (2017). 10.1126/scitranslmed.aah6500
