By Aila Berrigan
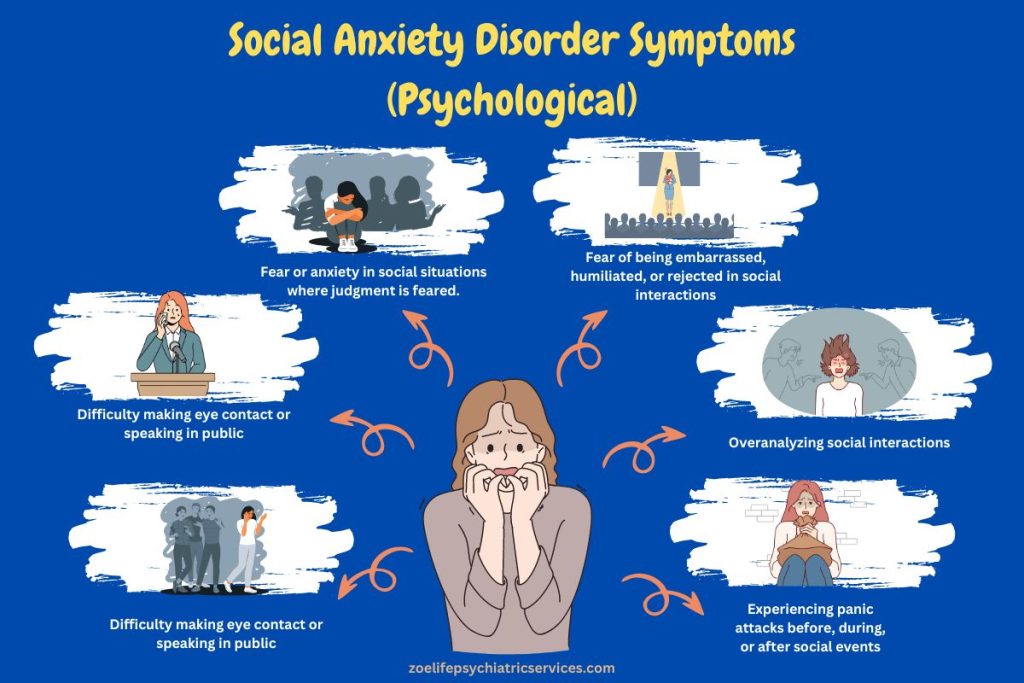
Figure 1. Infographic about social anxiety. Graphic from zoelife, 2024.
Introduction:
Ever wonder how much of an impact your gut microbiome really makes on everyday life? New research suggests your microbiome can affect your physical and emotional well being, including levels of social anxiety. “The gut microbiota shows compositional alterations in a variety of psychiatric disorders including depression, generalized anxiety disorder (GAD), autism spectrum disorder (ASD) and schizophrenia but studies investigating the gut microbiome in social anxiety disorder (SAD) are very limited” (Butler, 2023).Therefore researchers took it upon themselves to study the effects of our microbiome on social anxiety disorder. Social anxiety disorder has become one of the most common psychiatric conditions with rates as high as 13% (Butler, 2023). The current treatments for SAD are not always effective, “the use of psychosocial/psychotherapeutic approaches declines gradually from initiation of treatment over the course of 8 years” (Keller, 2003). This has encouraged researchers to look at alternative treatments which ultimately led them to dive deeper into our gut-brain axis. “It is broadly recognized that the gut and brain are in constant bidirectional communication, of which gut microbiota and its metabolic production are a major component, and form the so-called gut microbiome–brain axis” (Sasso, 2023). With this information they hope to be able to predict and treat SAD through understanding the microbes at play.

