It is currently estimated that the number of bacterial cells in our body roughly matches or exceeds the number of human cells, with the majority of these bacteria residing in the gut (Sender, et. al 2016). You may be familiar with literature identifying a “gut-brain” axis, i.e. a relationship between mental health and the composition of our microbiota. Studies have shown correlations between bacterial community makeup and disorders such as autism, depression and schizophrenia (Foster & Neufield 2013), (Dickerson, et. al 2017). Bacterial disbalance has also been correlated with diseases such as diabetes and obesity (Hartstra, et. al. 2014). A common factor between these disorders is that they are generally associated with lower microbial diversity. While there is a growing body of literature supporting the relationships between disease and dysbiosis, a perturbation of the microbial community, little research has explored the relationships between personality and patterns in variation of the healthy microbiome.

Enter Dr. Katrina Johnson of Oxford, who is especially interested in understanding how microbiota help to create the spectrum of human personality in the general population. To measure variation in personality, Johnson uses the “The Big Five” inventory which measures variation in personality using the following measures:
-
- Openness to experience (creativity, inclination to seek new experiences)
- Conscientiousness (organization, adherence to rules)
- Extroversion (seeking out the company of others)
- Agreeableness (cooperation in social settings, kindness, trust of others)
- Neuroticism (sensitivity to negative emotions)
Central Question:
Are we able to make predictions about personality through observing the patterns in composition of the gut microbiome? By pairing modern psychology with emerging technologies, like the widely available and easy to use at-home microbiome kit, Johnson is beginning to address this question.
Evidence:
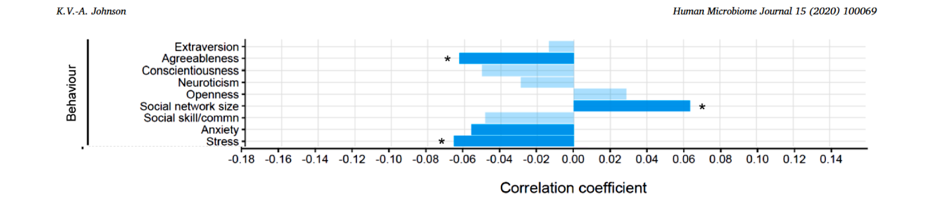
The above figure shows that trait agreeableness and propensity to experience stress were significantly correlated with decreased microbial diversity. Being a very agreeable person can increase stress, and thereby decrease diversity. Folks with higher trait agreeableness are less likely to barter for raises at work, more likely to be exploited and overcommit themselves, as well as placing their needs beneath the needs of others. (For further information, see video by psychologist Jordan Peterson.) These can all increase stress levels and thereby have an impact on diversity.
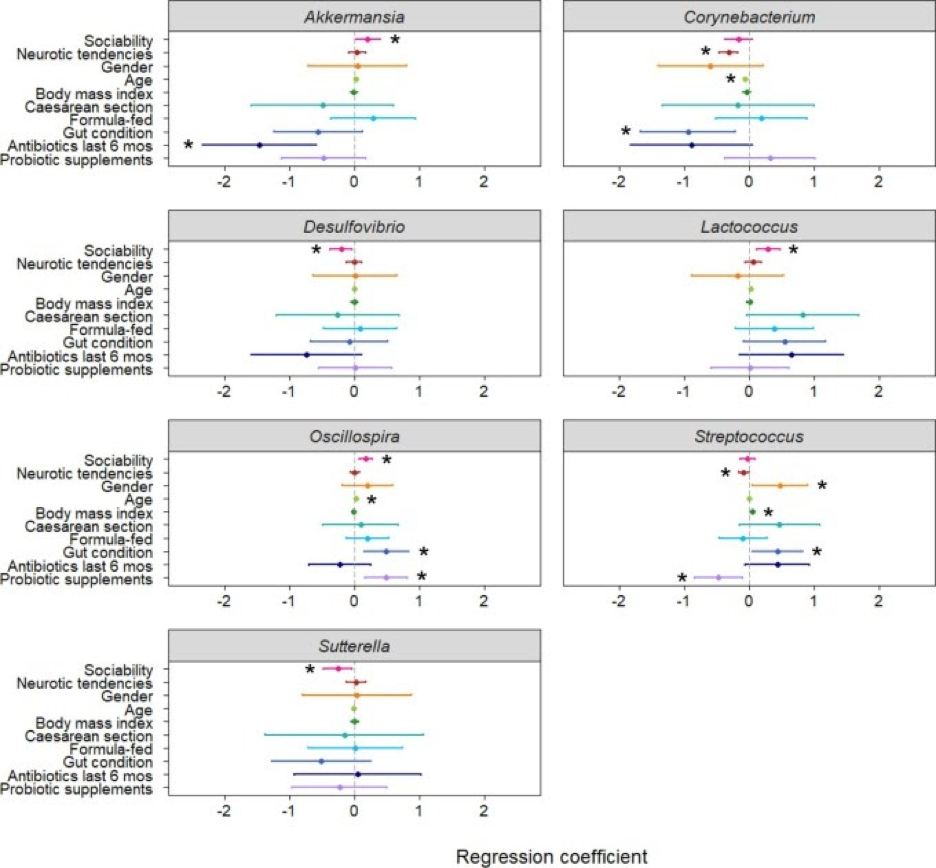
Johnson found that there is a positive correlation between microbial diversity and social network size; trait extraversion being an indicator of social network size. The genera Akkermansia, Lactococcus and Oscillospira were significantly more abundant in individuals that measured high in sociability. Johnson postulates that the protective effects against stress that a large social network provides could be a part of the relationship involved in this correlation. Interestingly, a previous study cited in the paper (Wang, et al., 2011) indicates that individuals with autism have significantly decreased levels of these same genera. Though, it is important to note that in animal studies Oscillospira was also correlated with group density and is a part of a genera that are known for producing spores that can be transmitted socially (Johnson), so it is possible that the correlation is actually driven by the transmissibility of the bacteria. Two genera, Desulfovibrio and Sutterella were found to be significantly more abundant in those with low sociability scores, and are also implicated in those with autism.
Individuals measuring high in trait neuroticism had significantly lower abundances of Corynebacterium and Streptococcus. High neuroticism is associated with an increased risk of developing depression, again indicating that patterns observed in the microbiome may be helpful in identifying and addressing mental illness. Johnson’s research also indicated that those considered “adventurous eaters” also had more diverse microbial communities. Openness to experience is measured by the trait openness, and therefore could also be predicted by microbial markers.
My Questions:
While we are able to identify a significant relationship between traits that determine sensitivity to stress and anxiety with microbial composition it is difficult to discern which direction the effect is in. While behavior can shape the microbiome, the microbiome can shape behavior; as scientists attempt to use the knowledge for therapeutic purposes it will be important to tease apart the details. Cohort studies designed around the specific mechanisms and pathways of the bacteria implicated in disease would be both interesting and instrumental in developing more holistic treatments of disease.
I would be interested to see the effects of increasing levels of deficient bacteria in those with identified illnesses. Fecal transplants have shown promise in the treatment of human dysbioses (Wischmeyer, et al. 2016), as research progresses I would also be very interested to see studies attempting to help those with mental illnesses such as autism and depression.
I also wonder if these patterns could be useful screening tools for diseases that are sometimes difficult to diagnose. Many screening tools for mental illness involve clinical assessment paired with patient questionnaires, but the ability to have microbial compositions biomarkers could be revolutionary in mental health screening.
Further Reading:
The Secret Power of Your Poo by Katerina Johnson
A video by the author discussing the potential for fecal matter transplants in treatment for diseases like obesity and autism.
A Gut Feeling by Nancy Averett
Breaking down the article in terms that are a bit easier to understand.
References:
Dickerson, Faith, Emily Severance and Robert Yolken. “The Microbiome, Immunity, and Schizophrenia and Bipolar Disorder.” Brain, Behavior, and Immunity, vol. 62, 2017, pp. 46–52. , https://doi.org/10.1016/j.bbi.2016.12.010
Foster, Jane A. and Karen-Anne Mcvey Neufeld. “Gut–Brain Axis: How the Microbiome Influences Anxiety and Depression.” Trends in Neurosciences, vol. 36, no. 5, 2013, pp. 305–312., https://doi.org/10.1016/j.tins.2013.01.005
Hartstra, Annick V., Kristien Bouter, Fredrik Bäckhed and Max Nieuwdorp. “Insights Into the Role of the Microbiome in Obesity and Type 2 Diabetes.” Diabetes Care, vol. 38, no. 1, 2014, pp. 159–165., https://doi.org/10.2337/dc14-0769
Johnson, Katerina V.-A. “Gut Microbiome Composition and Diversity Are Related to Human Personality Traits.” Human Microbiome Journal, vol. 15, 2020, p. 100069., https://doi.org/10.1016/j.humic.2019.100069
Sender, Ron, Shai Fuchs and Ron Milo. “Revised Estimates for the Number of Human and Bacteria Cells in the Body.” PLOS Biology, Public Library of Science, 2016, https://doi.org/10.1371/journal.pbio.1002533
Wang, Lv, Claus T. Christopherson, Michael J. Sorich, Jacobus P. Gerber, Manya T. Angley and Michael A. Conlon. “Low Relative Abundances of the Mucolytic Bacterium Akkermansia Muciniphila and Bifidobacterium Spp. in Feces of Children with Autism.” Applied and Environmental Microbiology, vol. 77, no. 18, 2011, pp. 6718–6721., https://doi.org/10.1128/AEM.05212-11
Wischmeyer, Paul E., Daniel McDonald and Rob Knight. “Role of the Microbiome, Probiotics, and ‘Dysbiosis Therapy’ in Critical Illness.” Current Opinion in Critical Care, vol. 22, no. 4, 2016, pp. 347–353., https://doi.org/10.1097/MCC.0000000000000321
