Background:
Between the years of 2010 and 2014 2,910,588 people died of cancer in the United States despite our best efforts to fight cancer with methods like chemotherapy and surgery (Howlader et al., 2017). While there are many reasons why cancers might prevail over our best efforts, a relatively common reason is the devolvement of chemotherapy resistance (Housman et al., 2014). This resistance can come in many forms; ranging from drug inactivation to changing the target site of the drug. In an attempt to combat resistance, chemotherapy drugs have been given out in cocktails containing multiple drugs that all work in a different way in the hope of killing all the resistant cells at once. This method was based off of the theory that while the mechanisms of resistance are known to be complex, the resistance always stems from cancer cells themselves. However this theory has been challenged in the last few years with the discovery that cancer cells could be protected from chemotherapy drugs by the normal cells (stroma) around the cancer cells (Feig et al., 2012; Klemm and Joyce, 2015).
One type of stroma that was identified as contributing to chemotherapy resistance was human dermal fibroblasts (HDFs)(Straussman et al., 2012). Human dermal fibroblasts are the cells that make the connective tissue that supports the outermost layer of skin. Further research showed that these cells secreted hepatocyte growth factor which might be the cause of the chemotherapy resistance, however not all of the cells had the ability to secrete this growth factor. Geller et al. started their study hoping to understand more about how the human dermal fibroblasts that could not secrete hepatocyte growth factor lead to the resistance of the chemotherapy drug gemcitabine in cancer cell (2017). Gemcitabine is a commonly used chemotherapy that is effective on many types of cancers. Geller et al. noticed that colorectal and pancreatic cancer cell lines grew in the presence of gemcitabine as long as their medium had at some point grown in HDFs. Thinking it was something in the medium, the researchers filtered the fibroblast conditioned medium and found that suddenly the resistance to gemcitabine was lost.
Central question:
What in the human dermal fibroblasts conditioned medium causes cancer cell lines to develop resistant to the chemotherapeutic drug gemcitabine?
Evidence:
Whole-genome sequencing of the conditioned medium found the DNA of the bacteria Mycoplasma hyorhinis. To test if the M. hyorhinis bacteria were the cause of the gemcitabine resistance, human dermal fibroblasts infected with M. hyorhinis were treated with antibiotics. These cells no longer conferred the gemcitabine resistance to the cancer lines, which was consistent with the hypothesis that M. hyorhinis was the cause of the gemcitabine resistance.
Next the researchers wanted to know if the resistance mechanism was limited to strictly M. hyorhinis. This was done by incubating gemcitabine in 27 different bacteria for 3 hours. After filtering, the gemcitabine was used to treat cancer cells lines. Of the 27 different bacteria tested, thirteen neutralized the gemcitabine thereby conferring resistance to the cancer cells. By analyzing the gemcitabine after it had been incubated with bacteria the researchers found that the gemcitabine was losing an important nitrogen group causing it to turn into 2’²,2’²-difluorodeoxyuridine which is not able to kill cancer cells. Looking at the bacterial strains that neutralized gemcitabine Geller et al. found that they all contained the eight hundred nucleotide long gene coding for the bacterial enzyme cytidine deaminase (CDD). Ninety eight percent of all bacteria containing this gene are of the bacterial class Gammaproteobacteria. To confirm that the CDD gene in the Gammaproteobacteria was responsible, the researchers took a E. coli, which naturally has the CDD gene, and created various strains which were missing a gene. Of all seven knock-outs, only the strain missing the CDD gene and the nupC gene (which codes for a transporter that is hypothesised to be used to import gemcitabine into the cell) caused the cancer cells to lose resistance to the gemcitabine.
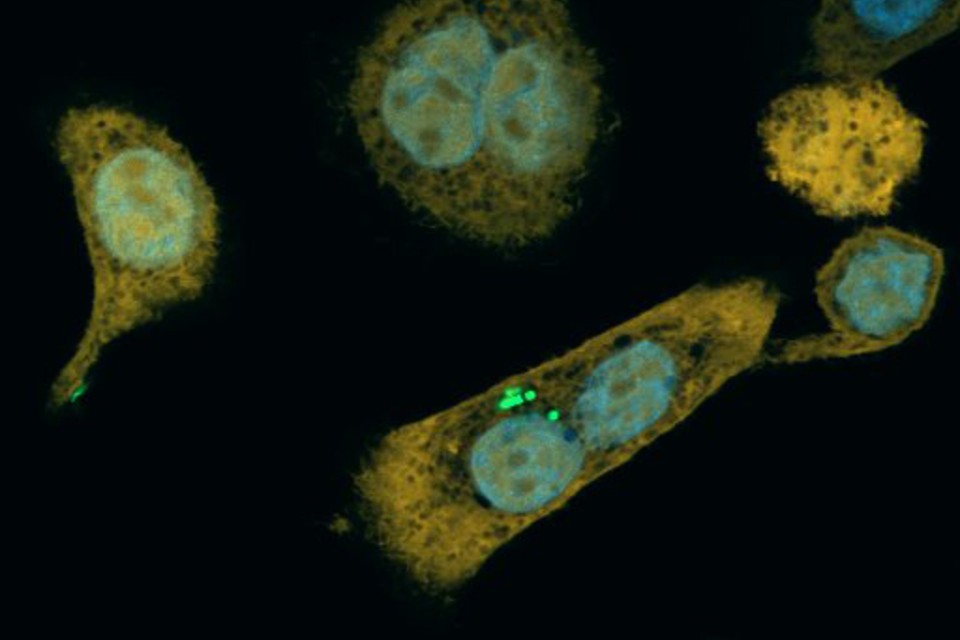
To see if their results would work in a living model, Geller et al. injected Gammaproteobacteria that had a bioluminescence gene into the tails of mice with colon cancer. Using the bioluminescence they showed that the bacteria preferentially colonized the tumor. The mice were then treated with either gemcitabine or gemcitabine and ciprofloxacin (an antibiotic). The mice treated with gemcitabine alone saw a fifteen fold increases in tumor size, while the mice treated with both gemcitabine and ciprofloxacin saw no increase in tumor size. Lastly the researchers did DNA tests on one hundred thirteen human pancreatic ductal adenocarcinoma as well as twenty normal pancreatic samples to see what microbes were present. Gammaproteobacteria were much more common in the pancreatic ductal adenocarcinomas with seventy six percent of the samples containing Gammaproteobacteria compared to only fifteen percent of the normal pancreatic samples.
Overall this study showed that Gammaproteobacteria colonize some cancerous tumors as well as their surrounding stroma in humans. Due to Gammaproteobacteria having the CDD gene, they can convert the chemotherapy drug gemcitabine to an inactive form, thereby protecting cancerous tumors (Geller et al., 2017).
Questions / Future research:
According to Geller et al. some Gammaproteobacteria conferred resistance to Oxaliplatin, another chemotherapy drug. However, resistance to Oxaliplatin was not due to the CDD gene as knock-out bacteria for the CDD gene still rendered the drug ineffective. The mechanism of resistance to Oxaliplatin might be interesting as this mechanism might also be be the cause of resistance to other chemotherapy drugs. Could these results be used in a clinical setting? While the results of these study could have clinical significance, the authors pointed out in a interview (see further reading) that the use of antibacterial drugs by a cancer patient could yield unwanted side effects due to the depletion of beneficial bacteria that exist all over our body and prevent unwanted pathogenic bacteria from taking host. Instead the authors suggested the development of a molecule that would inactivate the protein made by the CDD gene which the study found to be an important part in how bacteria inactivate the gemcitabine.
Since the Gammaproteobacteria seem to preferentially colonize the tumors it would be interesting to look into whether or not a chemotherapy drug could be developed that is injected in an inactive form and relies on the bacteria’s CDD gene to remove chemical groups and make it active. This would be extremely beneficial as it would allow for the drug to target cancer cells over regular cells thereby increasing the therapeutic index which signifies that the chemotherapy would be less dangerous and have less the side effects.
Further reading:
If you are interested in reading one of the press releases for this article as well as some of the comments that the authors of the study had on the topic and its usefulness in the clinical setting, The Atlantic has a good article titled How Bacteria Could Protect Tumors From Anticancer Drugs (Yong, 2017). Also if you are interested in how non-microbe related cancer resistance works compared to microbe antibacterial resistance there is an excellent paper by Lambert et al (2011).
References:
- Feig, C., Gopinathan, A., Neesse, A., Chan, D., Cook, N. and Tuveson, D. (2012). The Pancreas Cancer Microenvironment. Clinical Cancer Research, 18(16), pp.4266-4276. DOI:10.1158/1078-0432.CCR-11-3114
- Geller, L., Barzily-Rokni, M., Danino, T., Jonas, O., Shental, N., Nejman, D., Gavert, N., Zwang, Y., Cooper, Z., Shee, K., Thaiss, C., Reuben, A., Livny, J., Avraham, R., Frederick, D., Ligorio, M., Chatman, K., Johnston, S., Mosher, C., Brandis, A., Fuks, G., Gurbatri, C., Gopalakrishnan, V., Kim, M., Hurd, M., Katz, M., Fleming, J., Maitra, A., Smith, D., Skalak, M., Bu, J., Michaud, M., Trauger, S., Barshack, I., Golan, T., Sandbank, J., Flaherty, K., Mandinova, A., Garrett, W., Thayer, S., Ferrone, C., Huttenhower, C., Bhatia, S., Gevers, D., Wargo, J., Golub, T. and Straussman, R. (2017). Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science, 357(6356), pp.1156-1160. DOI:10.1126/science.aah5043
- Housman, G., Byler, S., Heerboth, S., Lapinska, K., Longacre, M., Snyder, N. and Sarkar, S. (2014). Drug Resistance in Cancer: An Overview. Cancers, 6(3), pp.1769-1792. DOI:10.3390/cancers6031769
- Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2014, National Cancer Institute. Bethesda, MD, Retrieved from link, based on November 2016 SEER data submission, posted to the SEER web site, April 2017.
- Klemm, F. and Joyce, J. (2015). Microenvironmental regulation of therapeutic response in cancer. Trends in Cell Biology, 25(4), pp.198-213. DOI: 10.1016/j.tcb.2014.11.006
- Lambert, G., Estévez-Salmeron, L., Oh, S., Liao, D., Emerson, B., Tlsty, T. and Austin, R. (2011). An analogy between the evolution of drug resistance in bacterial communities and malignant tissues. Nature Reviews Cancer, 11(5), pp.375-382. DOI:10.1038/nrc3039
- Straussman, R., Morikawa, T., Shee, K., Barzily-Rokni, M., Qian, Z., Du, J., Davis, A., Mongare, M., Gould, J., Frederick, D., Cooper, Z., Chapman, P., Solit, D., Ribas, A., Lo, R., Flaherty, K., Ogino, S., Wargo, J. and Golub, T. (2012). Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature, 487(7408), pp.500-504. DOI:10.1038/nature11183
- Yong, E. (2017). How Bacteria Could Protect Tumors From Anticancer Drugs. The Atlantic. Retrieved from link
