A little bit of background
What in the world is ADHD you might ask? ADHD stands for Attention Deficit/Hyperactivity Disorder and it is a common mental disorder that is found in school-aged children, but can also affect many adults (Parekh et al. 2017)! Symptoms of ADHD include inattention, impulsivity, and/or hyperactivity. If you have ever driven a vehicle without power-steering, you might have experienced the vehicle steering less sharply than what was intended by the driver. Some people describe their experience of having ADHD as if their brain is doing this! With ADHD, you might find yourself having to put in a lot more effort in a specific task just to avoid going off of the road.
There are treatments, such as stimulants and behavioral therapies available to address and help regulate the symptoms of ADHD. Although research is ongoing, there is no known cure for ADHD. Rather, just relief for the symptoms. However, researchers are starting to look into a different factor: the gut microbiome. Do inhabitants of our very own gut affect our mental health? They sure do! In fact, studies have been done that specifically look at connections between the microorganisms in our own intestines, also known as the gut microbiome, and ADHD!
Microorganisms are able to affect the brain through the use of the gut-brain axis. What the heck is a gut-brain axis? The gut-brain axis is a system in all of us. It includes signaling known as biochemical signaling, where your gastrointestinal tract can receive signals from your brain, and your brain can receive signals from your gastrointestinal tract, as shown in the image below. In other words, it’s how your gut and brain communicate with one another. The microbiota in our gut need to be able to communicate with us in order for the both of us to function properly. It’s their job to talk to us! This exchange can influence our homeostasis (internal balance) and health, and is done by biochemical signaling. Biochemical signaling can happen by three mechanisms: communication between neurons, the immune system, and endocrine signaling. These special mechanisms work together to create a communication network that can link hormone imbalances to neurodegeneration, which can include things like your metabolism and immune responses (Westfall et al. 2017).
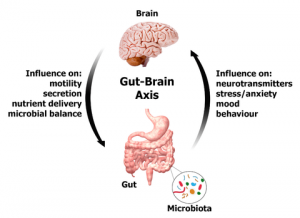
There are mediators in the brain that allow it to influence the gastrointestinal tract. An example of this can be when you’re stressed or too excited you may get a stomach ache or have diarrhea. In this way, the brain is reacting and sending out signals for what you are feeling, and the microbiota in your stomach are affected by this signaling, which ultimately affects their host: you. A previous study has looked at central nervous system dysfunctions and irritable bowel syndrome and claimed that psychiatric disorders that may arise as a result of stress, such as depression and anxiety, can occur concurrently with gastrointestinal issues (Yu et al. 2015). They often times go hand-in-hand.
Researchers are starting to recognize that our very own microbiome has a huge impact on our overall health, including mental health and brain function (Aarts et al 2017). This is possible because microorganisms that live in the gut are able to synthesize (make or produce) big brain chemicals called neurochemicals and also their precursors. Precursors are an important aspect of this study, as they are essential amino acids and some of them cannot be produced by the human body itself, but they are small enough to pass through the blood-brain-barrier. They are smaller chemical compounds that precede, or come before another bigger chemical compound in a metabolic pathway. Precursors can play a big part in a chemical reaction that produces another compound. New and increasing evidence is starting to come to the surface covering this topic everyday! Here, we’ll see what new research from Aarts et al. (2017) has to say about how the gut microbiome, which is present in all of us, may affect or even cause ADHD!
So, what is it, exactly, they’re trying to say here?
The big question being asked here is how exactly the gut microbiome can cause or affect ADHD. What are the gut microbiome differences between people with ADHD and healthy people? How does this difference relate to neural reward processing, or reward anticipation? What specific mechanisms come into play? I’m sure all of you are wondering. According to Aarts et al. (2017), it might have something to do with the gut-brain axis. Aarts et al. (2017) hypothesized that there would be a microbiome difference between people with ADHD and people who did not have ADHD, and that the differences in the microbial communities might be connect to why or how these people have ADHD.
Here’s the evidence
Aarts et al. (2017) found that there was a difference in the microbial community of the gastrointestinal tract in people who did have ADHD compared to the microbial community of the gastrointestinal tract in people who did not have ADHD. These researchers found an increased abundance of a bacteria, called Bifidobacterium, among people with ADHD. The phylum Actinobacteria was also more abundant in ADHD cases, but some bacteria known as Firmicutes were found to be at a lower abundance in ADHD cases. This was a strange discovery because Firmicutes, along with their friend Bacteroidetes, are the dominant microbial inhabitants of an average human gut.
In a similar study, Partty and her colleagues were able to show that a decrease in the genus Bifidobacterium present in three and six month old children resulted in ADHD or even Asperger syndrome by the age of 13 (Partty et al. 2015). Bifidobacterium is normally a pretty dominant species of microbe in a child’s gastrointestinal tract, so seeing a decrease in abundance of this species probably means that something is up.
Reward anticipation is a hallmark of ADHD. It is a special thing that provides an incentive; it’s where you expect a reward out of something and that induces motivation. You become motivated to get something done because you expect to get a reward out of doing the task. Dopamine is a neurotransmitter that is responsible for the brain’s reward and pleasure signals. Dopamine is thus linked to reward anticipation, so they go hand-in-hand. Precursors of Dopamine are the ones that can affect reward anticipation, because they are the chemicals that can pass through the blood-brain-barrier, monoamines such as Dopamine cannot.
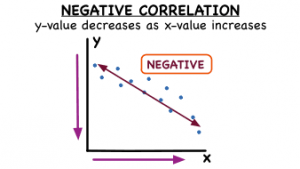
Aarts et al. (2017) also discovered a lot of information regarding the enzyme, Cyclohexadienyl Dehydratase (CDT). As mentioned before, the genus Bifidobacterium was found to be significantly more abundant in people with ADHD than people without ADHD. However, it doesn’t end there. The increase of this genus was found to be solely responsible for the increase in CDT. Now, CDT is known for producing a special essential amino acid, Phenylalanine. Since Phenylalanine is an essential amino acid, it cannot be made naturally by humans. Instead, it has to be made from outside sources, such as the food we eat or the microorganisms we house, so that it can be absorbed from the intestinal tract. However, this special little essential amino acid is actually a precursor of not only dopamine, but noradrenaline as well and it can cross the blood-brain-barrier! The neurotransmitters dopamine and noradrenaline are affected in people with ADHD. Dopamine modulates reward anticipation responses, and it was found that the CDT enzyme is negatively correlated with reward responses in the brain. Negative correlation is a relationship between two things, where one thing increases as the other decreases, and vice versa, as seen in the image below. In this case, the higher the levels of CDT someone has in their body, the less their brain is going to respond to reward.
The microbial community found in the gut may very well be responsible for increased levels of CDT, which is associated with phenylalanine availability. A result of this could be disturbed dopamine signaling and decreased reward responses in the ventral striatum in the brain. ADHD symptoms have been linked to significantly high levels of phenylalanine. Pretty weird, right?
Questions I have
After reading this article, I started to wonder if we could ever transport a person’s gut microbiome who doesn’t have ADHD into a person who does have ADHD? Would that help at all or have any effect? Are there other mental disorders we could look at, such as aspergers, or autism that the human microbiome could play a role in? Is the enzyme CDT solely responsible for the synthesis of phenylalanine? What other enzymes are there? Is phenylalanine the only precursor responsible for the negative correlation between increased levels of CDT and decreased levels of ventral striatal responses? What other factors could come into play?
Future possible experiments and studies
There are many possible studies and experiments that could be done from knowing how the gut microbiome plays a role in ADHD! Every new study brings about endless possibilities for further research, new ideas, and more experiments. Future studies could look at how the human gut microbiome could influence other mental disorders such as anxiety, post-traumatic stress disorder, depression, psychosis, and schizophrenia. A similar trend of how the gut microbiota influences the brain could be seen in other mental disorders, or it could be a totally different trend. Another interesting topic to look at would be early detection in these disorders and illnesses and see if there is a way to alter a young person’s gut microbiota in such a way as to prevent the disorder or illness altogether, or at least relieve the symptoms so that there would be no need for medication.
For more information
- If you would like to find out more regarding ADHD, the causes of ADHD, or ADHD in children and adults, click here.
- If you would like to learn more about the gut-brain axis, how it works and how it is related to this study, click here.
- As it was not mentioned much in this post, you can find more information regarding the blood-brain-barrier and how it all works here.
References
- Aarts, E., T.H.A. Ederveen, J. Naaijen, M.P. Zwiers, J. Boekhorst, H.M. Timmerman, S.P. Smeekens, M.G. Netea, J.K. Buitelaar, B. Franke, S.A.F.T. van Jijum, and A.A. Vasquez. 2017. Gut microbiome in ADHD and its relation to neural reward anticipation. PLoS ONE 12(9): 1-17. https://doi.org/10.1371/journal.pone.0183509
- Partty, A., M. Kalliomaki, P. Wacklin, S. Salminen, and E. Isolauri. 2015. A possible link between early probiotic intervention and the risk of neuropsychiatric disorders later in childhood: a randomized trial. Pediatric research 77(6): 823-828. https://doi.org/10.1038/pr.2015.51
- Westfall, S., N. Lomis, I. Kahouli, S.Y. Dia, S.P. Singh, and S. Prakash. 2017. Microbiome, probiotics and neurodegenerative diseases: deciphering the gut brain axis. Cell and Molecular Life Sciences 74: 3769-3787. https://doi.org/10.1007/s00018-017-2550-9
- Yu, Y., S. Wu, J. Li, R. Wang, X. Xie, X. Yu, J. Pan, Y. Xu, and L. Zheng. 2015. The effect of curcumin on the brain-gut axis in rat model of irritable bowel syndrome: involvement of 5-HT-dependent signaling. Metabolic Brain Disease 30: 47-55. https://doi.org/10.1007/s11011-014-9554-z
- Parekh, R. 2017. What is ADHD? American Psychiatric Association. https://www.psychiatry.org/patients-families/adhd/what-is-adhd
- Rege, S., and J. Graham. 2017. The Simplified Guide to the Gut-Brain Axis – How the Gut and and the Brain Talk to Each Other. https://psychscenehub.com/psychinsights/the-simplified-guide-to-the-gut-brain-axis/
