Background
Ambulances are in almost every city in the United States. Depending on the city and service, ambulances can go on over a dozen calls a day. With each call and patient, healthcare workers and ambulance surfaces are exposed to new organisms. EMS (Emergency Medical Services) providers are constantly treating and transporting patients with viral infections and bacterial infections, trauma patients with open wounds, and patients with weak immune systems, such as young children and elderly (Caroline, 2013). Depending on the service, certain ambulances might get a higher population of patients with weakened immune systems than others, or more patients that have spent prolonged periods of time in hospitals.

After each patient the ambulance is cleaned and thoroughly disinfected. Surfaces are sprayed with cleaning solutions and wiped down. These surfaces include the gurney, bench seat, monitor and monitor probes, action area, floor, specific equipment, and any other surfaces that might have come into primary, secondary, or even tertiary contact with the patient. All sheets/fabrics that have come into contact with the patient are replaced. Many of these sites were examined over the duration of a study by O’Hara and a team of researchers.
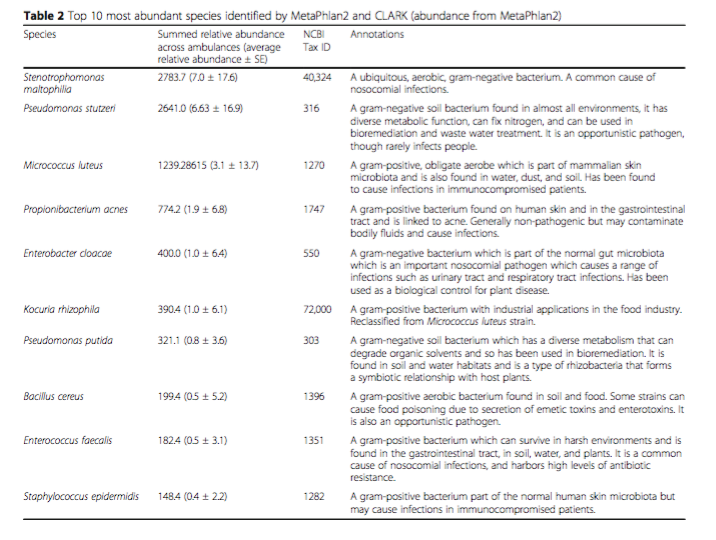
Some of the most ubiquitous bacteria found in ambulances across the US (according to the study) are: Stenotrophomonas maltophilia, Pseudomonas stutzeri, Micrococcus luteus, Propionibacterium acnes. All of these, with the exception of Pseudomonas stutzeri, commonly cause infections in susceptible patients (O’Hara et al. 2017). The fact that these bacteria are commonly present is particularly concerning as these patients will be going to hospitals where nurses and doctors may be the next vectors to spread these infectious bacteria.
Question
What kinds of microorganisms are in ambulances across the United States?
Evidence
398 swabs were taken from multiple surfaces found inside of an ambulance. These included places such the bench seat, monitor, AED, stethoscope, and rear light control panel. They used whole-genome shotgun sequencing to identify the species of microorganisms that were present. Whole genome shotgun sequencing essentially means that the DNA from all organisms present are broken up into random fragments. These are then sequenced and then put back together by piecing together the sequences that overlap. Through this method, scientists are able to sequence a large amount of DNA.
When analyzing the DNA, the sequences were run through two different programs to ensure accuracy. For the purposes of the study it was extremely important to negate any false positives that may have otherwise occurred. Due to this, organisms that may have been present may not have been identified with certainty. Further studies may be necessary to identify further organisms present.
What they found is that there were a significant number of microbes present that were associated with both skin and blood on various surfaces. Many of these organisms were linked to HAIs (Hospital Acquired Infections). Some of the bacteria were found to cause infections in immunocompromised patients and some were benign. Sites with the greatest numbers of microbes include the stethoscope and rear light control panel. Other surfaces, such as the monitor and stretcher, had high readings as well.
My Questions
In future studies, I would like to look more at the medics themselves. Throughout a shift medics can see multiple patients a day. Though the back of the ambulance gets cleaned with every patient, EMS workers do not often have the time or ability to change into clean uniforms. Many stations, particularly in private EMS, do not have stations set up with showers. In stations that do have showers, EMS often get calls to frequently to be able to enjoy them.
I would like to know how many and what kinds of microorganisms are present on EMS workers over the duration of a shift. Does it change? If so, how drastically? If medics see a significant number of patients a day and are only able to wash their hands between patients, is there any EMS worker to patient spread of microorganisms? How does this compare to the possible patient to Medic spread of organisms? Would there be more net movement of organisms to or from the patient?
Another consideration is to the quarters in which Medics sleep. Many services and departments have 24-hour shifts where medics are respondable. Depending on the service, medics may be expected to return to their stations when not on call for a period of time from evening to morning. During this time, EMS workers stay in their station between calls and try to sleep. Due to the nature of the career, EMS personnel are expected to be en route preferably under one minute . This means that many personnel sleep in their uniforms in order to be more prepared should a call come in. I would be curious to see a study done that investigates the organism diversity of living quarters, specifically bunk rooms, to the organisms regularly found in the ambulance.
Many departments are Fire and Emergency Medical Services. This means that the majority of firefighters are also EMTs, and as such are expected to cross-staff different rigs. I would like to see if there is significant transfer of microorganisms between rigs. In a fire engine or ladder truck, particular attention is not often paid to disinfect the cabs, as they are not considered to have significant contact with patients. This is in heavy contrast with ambulances with are disinfected thoroughly every day. As a result, I wonder if organisms are transferred between rigs, and how long these organisms might be present in each rig considering the differing rates of decontamination.
Another type of emergency transport service, very similar to ambulances, are medevac planes. These are staffed by MICPs (Mobile Intensive Care Paramedics) and Nurses. Patients are transported between hospitals, often from a smaller hospital to a larger more specialized hospital. These planes can also work as 911 responders, flying into villages and rural communities with the intent to stabilize and treat the patient. Patients can spend anywhere from minutes to hours in these planes depending on the destination. Due to this prolonged period of time, I wonder if there is an increased transmission of microorganisms. Are the organisms found in a plane similar to those found in an ambulance?
Additional Material
If interested in this subject, I would highly recommend looking at these other articles. They talk about the practices of healthcare workers as they relate to decontamination after patient care, and take a closer look at Hospital Acquired Infections (HAI’s).
Hand washing in Healthcare Workers
Ambulance Decontamination
Reducing the Incidence of Hospital Acquired Infections
HAI’s and How to Prevent Them
References
- Caroline, Nancy. “Emergency Care in the Streets (Seventh Edition).’ American Academy of Orthopaedic Surgeons (AAOS). Jones and Bartlett Learning Copyright 2013.
- Curos. “Hospital Acquired Infections and How to Avoid Them’. Curos Disinfecting Port Protectors. November 4, 2014. https://www.youtube.com/watch?v=izxdrkJIhQ4
- D.Pittet. “Compliance with hand disinfection and its impact on hospital-acquired infections’. Journal of Hospital Infection. Volume 48, Supplement A, August 2001, Pages S40-S46. https://doi.org/10.1016/S0195-6701(01)90012-X.
- Edmond, M. B., Wenzel, R. P. “The impact of hospital-acquired bloodstream infections.’ EmergInfect Dis. 2001 Mar-Apr; 7(2): 174—177. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2631709/
- O’Hara et al. “Metagenomic characterization of ambulances across the USA’. Microbiome (2017) 5:125. DOI 10.1186/s40168-017-0339-6
- “Reducing the Risk of Hospital Acquired Infections’. UCLA Health. Jan 9, 2015. https://www.youtube.com/watch?v=QIS8u6JEWEA
- University Fire Department. “Exposure Control Plan’ (Standard Operating Procedures). Signed November 2017.
