Background
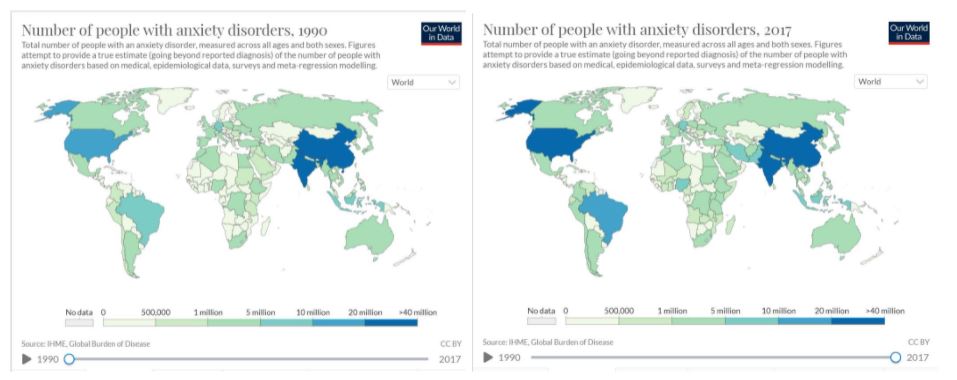
Mental health diseases like depression and anxiety have plagued humans presumably since we achieved sentience, and lately it seems like the mental health crisis in America is getting worse and worse. Everyone blames this rise on something different; social media, the pandemic, tumultuous politics, or just the dramatics of younger generations. No matter where the blame is placed, statistics show that the rise in the number of diagnoses is real. Almost all mental health diseases show growth, but anxiety and depression have skyrocketed (ADAA). Even before the COVID 19 pandemic, anxiety was at an all time high, as shown in the figure below.
Recent research has been exploring the link between mental health and the human microbiome. The microbes living within us have more influence on our systems than we ever imagined. From how we extract nutrients from food, to the ways our immune system reacts to intruders (Vangoitsenhoven, 2020), our microbes shape our bodies. They might also play a role in influencing thoughts and behavior. As we discover more links between physical and mental health, it seems more and more likely that microbes may have some effect on our mental wellbeing.
Scientists have begun to uncover a strong association between oral and mental health. One study found that people with severe mental illness were 2.7 times more likely to lose all their teeth than healthy people (Kisely, 2016). It has been speculated that this is because people with mental illness may care less about hygiene, or be more likely to use drugs and tobacco (Kisely, 2016).
In 2020, a group of researchers tried to find a deeper connection. They acknowledged that mental health may have more direct impacts on oral health than just poor hygiene. Stress triggers cortisol release, which builds up in the saliva. It also has ties to inflammation, which may exacerbate pre-existing oral diseases.
Central Question
What microbes and metabolites mediate the connection between the oral microbiome and adolescent depression and anxiety?
The Evidence (Simpson et al, 2020)
The 66 participants were 14-18 years old. Mental health symptom information was gathered using two questionnaires: one for depression (CESD) and one for anxiety (SCAS). Oral health information was also gathered with a questionnaire.
This study found that adolescents with depression or anxiety had a few distinct markers that separated them from healthy individuals- namely the composition of their microbiome. It reaffirmed what previous studies had found: that their saliva contained higher levels of cortisol and C-reactive proteins (CRPs). CRPs levels rise in response to inflammation. They also found that there were no significant differences in alpha or beta diversity between the mild and severe groups.
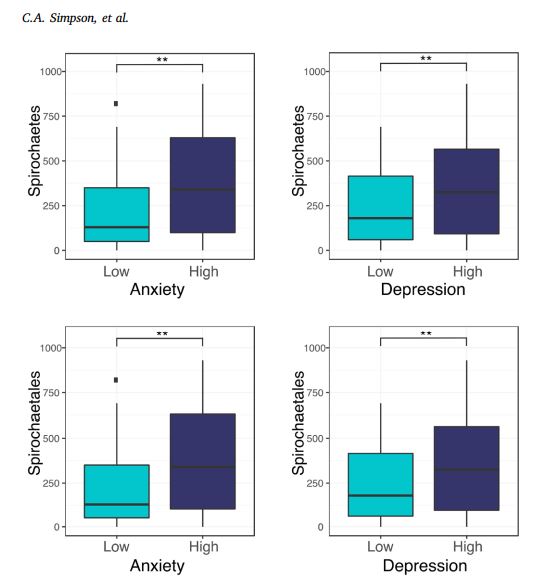
Individuals with depression and/or anxiety were also found to have abnormally high levels of taxa Spirochaetes and Spirochaetales. These taxa range from harmless to deadly, are members are responsible for syphilis, lyme disease, and other illnesses. Some taxa within these groups are also known to form biofilms and cause tissue damage. The quantity of these microbes increased with severity of the mental health disease; individuals with the most severe anxiety and depression had the highest levels of Spirochaetes and Spirochaetales. This abundance was not correlated with cortisol or CRP levels.
The graph below (fig. 2) shows how the target population differed between the groups. Those with high anxiety and depression had, on average, more than double the number of spirochaetales than those with low depression and anxiety.
The taxon Treponema was identified within the Spirocheatea family. While it didn’t account for the total increase in Spirochaetes, it was deemed significant due to its correlation with depression symptoms. Oral treponemes are known to rely on the catalysis of amino acids, which they get from host cells. This causes damage to the affected tissues. Treponema species have already been identified as playing roles in many serious oral diseases, such as peridontitis and endodontic infections.
My Questions
Within the article the authors note that they were unsure how the relationship between mental health and Spirochaetes was mediated, since they did not seem to be related to cortisol or CRP. More research is needed to determine the role Spirochaetes play in anxiety and depression. Will other studies find the same correlation? I would also like to investigate the accuracy of their original data. The oral health data was all self reported by the participants. A comprehensive oral exam by a professional would have provided more accurate and specific data. Conditions like anxiety and depression can affect pain perception (Kisely, 2016), leading participants to rate oral health inaccurately.
After reading this article, I would be interested to know how dental and mental health professionals can work together to treat an individual. Since the fields seem to go hand in hand, should it be the norm for psychiatrists to consult with dental professionals when treating those with anxiety or depression?
I would assume that the thought of expensive or painful dental work would increase symptoms in people with depression and anxiety. In turn, that may make oral health even worse. It would also be interesting to see a study that looks at the possibility of a positive feedback cycle in the mental/oral health scene. It seems like it may be an unfortunate cycle that should be addressed when treating patients who have both mental and oral diseases.
Further Reading
For more information on oral and mental health:
- No Mental Health without Oral Health This paper is from 2016, but it succinctly sums up what was known at the time about the mental and dental relationship.
For more information on depression and anxiety trends:
- Trends in Mood and Anxiety Symptoms and Suicide-Related Outcomes Among U.S. Undergraduates, 2007–2018: Evidence From Two National Surveys Gives information on undergrad mental health trends compiled from survey data.
- Mental Health A great site that provides graphs and infographics for a wide range of statistics.
References
Dattani, S. Ritchie, H. Roser, M. “Mental Health.” Our World in Data (2021), https://ourworldindata.org/mental-health.
“Facts & Statistics: Anxiety and Depression Association of America.” ADAA https://adaa.org/understanding-anxiety/facts-statistics.
Kisely, S. No Mental Health Without Oral Health. Can J Psychiatry (2016) 61(5): 277-282 doi: 10.1177/0706743716632523
Simpson, C., Adler, C., du Plessis, M., Landau, E., Dashper, S., Reynolds, E., Schwartz, O., Simmons, J. Oral microbiome composition, but not diversity, is associated with adolescent anxiety and depression symptoms. Physiology and Behavior 226 (2020) 113126 doi: 10.1016/j.physbeh.2020.113126
Vangoitsenhoven, R. and Cresci, G.A.M. Role of Microbiome and Antibiotics in Autoimmune Diseases. Nutrition in Clinical Practice, (2020) 35: 406-416. doi: 10.1002/ncp.10489
